Role of multidetector computed tomography in differentiating benign and malignant common bile duct strictures
Main Article Content
Abstract
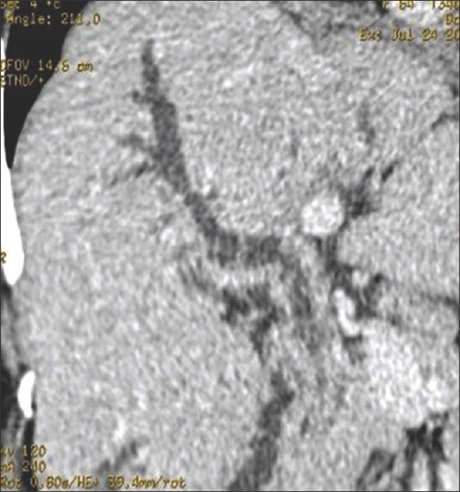
Objective: To evaluate the diagnostic features in differentiating malignant from benign common bile duct (CBD) strictures using contrast-enhanced multidetector computed tomography (MDCT).
Patients and Methods: An ambispective study from January 1, 2008 to December 31, 2010, on fifty patients with liver function tests suggestive of obstructive jaundice and an ultrasound showing biliary obstruction were included. A nonenhanced computed tomography (CT) was done before the administration of the contrast medium and then scans were routinely obtained in four phases: early arterial , late arterial, portal venous, and delayed phases. The CT scans acquired were reviewed on a picture archiving and communication system workstation. CT findings were interpreted with regard to wall thickness, the location, length involved,
enhancement pattern, presence of invasion, and margins of the stricture. These were compared with the attenuation of the normal CBD wall, the maximum CBD diameter proximal, and pancreatic duct dilatation.
Results: The mean age ± standard deviation of patients was 62.84 ± 11.61 years (range: 38–82 years). Among the fifty patients included in the study, 31 (62%) had malignant CBD stricture. The involved segments of malignant CBD strictures were significantly longer with significantly larger maximum proximal CBD diameter, considerably thicker and irregular stricture wall and showing more enhancement during delayed phase. No significant differences were found between malignant and benign CBD strictures with respect to stricture location.
Conclusions: Presence of irregular margins, invasion into neighboring tissues, long-segment involvement, more proximal CBD dilatation, and hyperenhancement in delayed and portal venous phases in contrast-enhanced MDCT helps in the differentiation of malignant from benign CBD strictures.
Downloads
Article Details
Section

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
How to Cite
References
1. Rösch T, Meining A, Frühmorgen S, Zillinger C, Schusdziarra V, Hellerhoff K, et al. A prospective comparison of the diagnostic accuracy of ERCP, MRCP, CT, and EUS in biliary strictures. Gastrointest Endosc 2002;55:870‑6.
2. Dadhwal US, Kumar V. Benign bile duct strictures. Med J Armed Forces India 2012;68:299‑303.
3. Darwish AN, El Fert AA, El Badry AM, Mousa E. Evaluation of the role of multidetector computed tomography in biliary obstruction. Tanta Med J 2013;41:318‑26.
4. Gerber S, Schweizer W. Surgical therapy of juxtapapillary tumors. Swiss Surg 2000;6:271‑4.
5. Chang S, Lim JH, Choi D, Kim SK, Lee WJ. Differentiation of ampullary tumor from benign papillary stricture by thin‑section multidetector CT. Abdom Imaging 2008;33:457‑62.
6. Yoon KH, Ha HK, Kim MH, Seo DW, Kim CG, Bang SW, et al. Biliary stricture caused by blunt abdominal trauma: Clinical and radiologic features in five patients. Radiology 1998;207:737‑41.
7. Han JK, Choi BI, Kim TK, Kim SW, Han MC, Yeon KM, et al. Hilar cholangiocarcinoma: Thin‑section spiral CT findings with cholangiographic correlation. Radiographics 1997;17:1475‑85.
8. Kim MJ, Mitchell DG, Ito K, Outwater EK. Biliary dilatation: Differentiation of benign from malignant causes – Value of adding conventional MR imaging to MR cholangiopancreatography. Radiology 2000;214:173‑81.
9. Al‑Mofleh IA, Aljebreen AM, Al‑Amri SM, Al‑Rashed RS, Al‑Faleh FZ, Al‑Freihi HM, et al. Biochemical and radiological predictors of malignant biliary strictures. World J Gastroenterol 2004;10:1504‑7.
10. Saluja SS, Sharma R, Pal S, Sahni P, Chattopadhyay TK. Differentiation between benign and malignant hilar obstructions using laboratory
and radiological investigations: A prospective study. HPB (Oxford) 2007;9:373‑82.
11. Kim HC, Park SH, Park SI, Shin HC, Park SJ, Kim HH, et al angiography. Acta Radiol 1992;33:351‑5.
12. Soto JA, Alvarez O, Lopera JE, Múnera F, Restrepo JC, Correa G, et al. Biliary obstruction: Findings at MR cholangiography and
cross‑sectional MR imaging. Radiographics 2000;20:353‑66.
13. Yeh BM, Liu PS, Soto JA, Corvera CA, Hussain HK. MR imaging and CT of the biliary tract. Radiographics 2009;29:1669‑88.
14. Inui K, Yoshino J, Miyoshi H. Differential diagnosis and treatment of biliary strictures. Clin Gastroenterol Hepatol 2009;7:S79‑83.
15. Akamatsu N, Sugawara Y, Osada H, Okada T, Itoyama S, Komagome M, et al. Diagnostic accuracy of multidetector‑row computed tomography for hilar cholangiocarcinoma. J Gastroenterol Hepatol 2010;14:1‑4.