Radiotherapy treatment of spinal metastases in Ibadan: A 9‑year review
Main Article Content
Abstract
Background: Metastatic spinal tumors signify disease progression and result in poor quality of life of patients. We are likely to see an increasing burden of spinal metastases due to the global trend of increasing cancer survival.
Objective: The objective of this study was to review the pattern of presentation and radiotherapy of metastatic spinal tumors in the Radiation Oncology Department, University College Hospital, Ibadan, Nigeria.
Materials and Methods: The radiation therapy records of all patients who received spinal irradiation between January 2007 and December 2015 were retrieved. The extracted data are patients’ sociodemographic, clinicopathologic, and treatment factors which include the radiation dose given and retreatment dose.
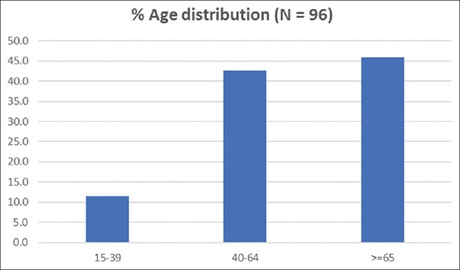
Results: Majority (91.7%) of the patients who had radiotherapy to the spine had metastatic spinal tumors. Male patients accounted for 69.1% of the cases and females accounted for 30.1% resulting in a male–female ratio of 2.23:1. Close to half (45.8%) of the patients were elderly. Prostate cancer (57.3%) and breast cancer (18.8%) were the most common primary sites. The most common involved spinal site was the thoracic region. In all age groups, fewer patients received a short radiotherapy treatment course (totaling 15 Gy or less and within a duration of 1 week) versus long radiotherapy treatment course (other radiation schedules not meeting criteria for short).
Conclusion: A high index of suspicion of metastatic spinal cancer is required, particularly for breast and prostate cancers. The authors recommend that more elderly patients should be treated with short-course radiotherapy.
Downloads
Article Details
Section
How to Cite
References
1. Joaquim AF, Powers A, Laufer I, Bilsky MH. An update in the management of spinal metastases. Arq Neuropsiquiatr 2015;73:795‑802.
2. Fact Sheets by Population. Available from: http://globocan.iarc.fr/Pages/fact_sheets_population.aspx. [Last accessed on 2015 Aug 13].
3. Wong DA, Fornasier VL, MacNab I. Spinal metastases: The obvious, the occult, and the impostors. Spine (Phila Pa 1976) 1990;15:1‑4.
4. Ortiz Gómez JA. The incidence of vertebral body metastases. Int Orthop 1995;19:309‑11.
5. Rades D, Fehlauer F, Veninga T, Stalpers LJ, Basic H, Hoskin PJ, et al. Functional outcome and survival after radiotherapy of metastatic spinal
cord compression in patients with cancer of unknown primary. Int J Radiat Oncol Biol Phys 2007;67:532‑7.
6. Delank KS, Wendtner C, Eich HT, Eysel P. The treatment of spinal metastases. Dtsch Arztebl Int 2011;108:71‑9.
7. Rougraff BT, Kneisl JS, Simon MA. Skeletal metastases of unknown origin. A prospective study of a diagnostic strategy. J Bone Joint Surg Am 1993;75:1276‑81.
8. Rades D, Conde AJ, Garcia R, Cacicedo J, Segedin B, Perpar A, et al. A new instrument for estimation of survival in elderly patients
irradiated for metastatic spinal cord compression from breast cancer. Radiat Oncol 2015;10:173.
9. Spinal Metastasis: Background, Pathophysiology, Prognosis; 06 December, 2017. Available from: https://emedicine.medscape.com/article/1157987‑overview. [Last accessed on 2017 Dec 23].
10. Bilsky MH, Lis E, Raizer J, Lee H, Boland P. The diagnosis and treatment of metastatic spinal tumor. Oncologist 1999;4:459‑69.
11. Boström A, Kanther NC, Grote A, Boström J. Management and outcome in adult intramedullary spinal cord tumours: A 20‑year single institution experience. BMC Res Notes 2014;7:908.
12. Rades D, Blach M, Nerreter V, Bremer M, Karstens JH. Metastatic spinal cord compression. Influence of time between onset of motoric
deficits and start of irradiation on therapeutic effect. Strahlenther Onkol 1999;175:378‑81.
13. Katagiri H, Takahashi M, Inagaki J, Kobayashi H, Sugiura H, Yamamura S, et al. Clinical results of nonsurgical treatment for spinal metastases. Int J Radiat Oncol Biol Phys 1998;42:1127‑32.
14. Popoola AO, Igwilo I, Sowunmi A, Ketiku K, Duncan KJ. Analysis of malignant spinal cord compression patients treated in a radiotherapy centre. Sch J Appl Med Sci 2013;1:906‑10.
15. Ciftdemir M, Kaya M, Selcuk E, Yalniz E. Tumors of the spine. World J Orthop 2016;7:109‑16.
16. Maranzano E, Latini P, Perrucci E, Beneventi S, Lupattelli M, Corgna E. Short‑course radiotherapy (8 Gy x 2) in metastatic spinal cord compression: An effective and feasible treatment. Int J Radiat Oncol Biol Phys 1997;38:1037‑44.
17. Sioutos PJ, Arbit E, Meshulam CF, Galicich JH. Spinal metastases from solid tumors. Analysis of factors affecting survival. Cancer 1995;76:1453‑9.
18. Dawotola DA, Odigie VI, Yusufu LM, Adamu A, Abur P, Jimoh AO, et al. External beam radiotherapy in metastatic bone pain from solid
tumours in Zaria Nigeria. Niger J Surg 2011;17:11‑4.
19. Maranzano E, Latini P. Effectiveness of radiation therapy without surgery in metastatic spinal cord compression: Final results from a
prospective trial. Int J Radiat Oncol Biol Phys 1995;32:959‑67.
20. Vincenzi B, Frezza AM, Schiavon G, Santini D, Dileo P, Silletta M, et al. Bone metastases in soft tissue sarcoma: A survey of natural history, prognostic value and treatment options. Clin Sarcoma Res 2013;3:6.
21. Yoshikawa H, Ueda T, Mori S, Araki N, Kuratsu S, Uchida A, et al. Skeletal metastases from soft‑tissue sarcomas. Incidence, patterns, and radiological features. J Bone Joint Surg Br 1997;79:548‑52.
22. Schiff D, O’Neill BP. Intramedullary spinal cord metastases: Clinical features and treatment outcome. Neurology 1996;47:906‑12.
23. Okeke LI, Ikuerowo SO, Popoola AA, Shittu OB, Olapade‑Olaopa EO. Clinical presentation and outcome of management of patients with
symptomatic spinal metastasis from prostate cancer: A five‑year experience. Afr J Urol 2006;12:134‑8.
24. Adewuyi SA, Chom ND, Humera M, Samaila MOA. Pattern of skeletal metastases from breast cancer in an Asian population. Niger J Surg Res 2006;8:128‑31.
25. Popoola AO, Igwilo AI, Sowunmi A, Ketiku KK, Duncan KJ, Hou N, et al. Pattern of bone metastasis in breast cancer patients at a radiotherapy facility in Lagos. Br J Med Med Res 2014;4:843.
26. Wilartratsami S, Muangsomboon S, Benjarassameroj S, Phimolsarnti R, Chavasiri C, Luksanapruksa P. Prevalence of primary spinal tumors: 15‑year data from Siriraj Hospital. J Med Assoc Thai 2014;97 Suppl 9:S83‑7.